Diabetic Neuropathy:
Can Diabetic Neuropathy be reversed: How to prevent it. The answer to reversal will be clear as this article explores what this complication is. First, let’s do a little digging and get a comprehensive understanding.
Individuals with diabetes are in great danger of various health problems such as:
Heart problem
Strokes
Eye Disease – Possible Blindness
Nerve Damage – Neuropathy
Amputation of foot or leg
Kidney Problems
Gum Disease
Loss of teeth
Another health problem related to diabetes includes the feet, as diabetes is among the major causes of lower limb amputation.
Amputation is undoubtedly the last resort concerning foot problems; however, it is surprising how a small cut or abrasion can lead to such dramatic outcomes.
Why is the Foot at Risk?
Relentless high blood glucose levels can eventually damage the body’s nerves, triggering a loss of sensation. Nerve damage can also cause pain in the hands, arms, and legs, causing problems in people’s everyday lives.
Your primary care service provider or Podiatrist must inspect your feet every year, consisting of a sensory examination to check for loss of feeling.
Without little cuts or abrasions, the neuropathic foot can go unnoticed. However, the injury can quickly become contaminated, leading to an infected ulcer, and might eventually result in the loss of the lower limb. Therefore, the significance of regular foot checks, foot care & diabetes can not be overlooked.
High-Risk Factors Leading to Diabetic Foot Ulcers
Some diabetic patients develop foot ulcerations, a few of which may result in amputation. The diabetic foot is at a greater danger of ulceration if other conditions are present such as vascular illness or peripheral neuropathy. However, numerous other factors can increase the risk of ulcers, such as: –
Cold feet or absent foot pulses
History of Foot Problems
Foot Deformities
Minimal mobility
Poor circulation
Inappropriate shoes
Unchecked blood glucose levels
A pain-free abrasion or corn can gradually advance to a traumatic foot ulcer, and if left unattended, skin degeneration might happen.
The primary purpose of this article, however, is to discuss one of the significant complications of diabetes that often precedes foot problems in diabetics, with a view on how to prevent or possibly reverse it.
Do you know that Diabetic Neuropathy is one of the most common complications of diabetes? Sadly, most diabetics don’t even understand what it is and how to prevent it until it becomes an issue.
This post will break it down and assist you in comprehending how to prevent this severe and possibly debilitating condition.
So, stay tuned as we address nine crucial questions to help you understand and avoid diabetic neuropathy.
But first, what are the risk factors?
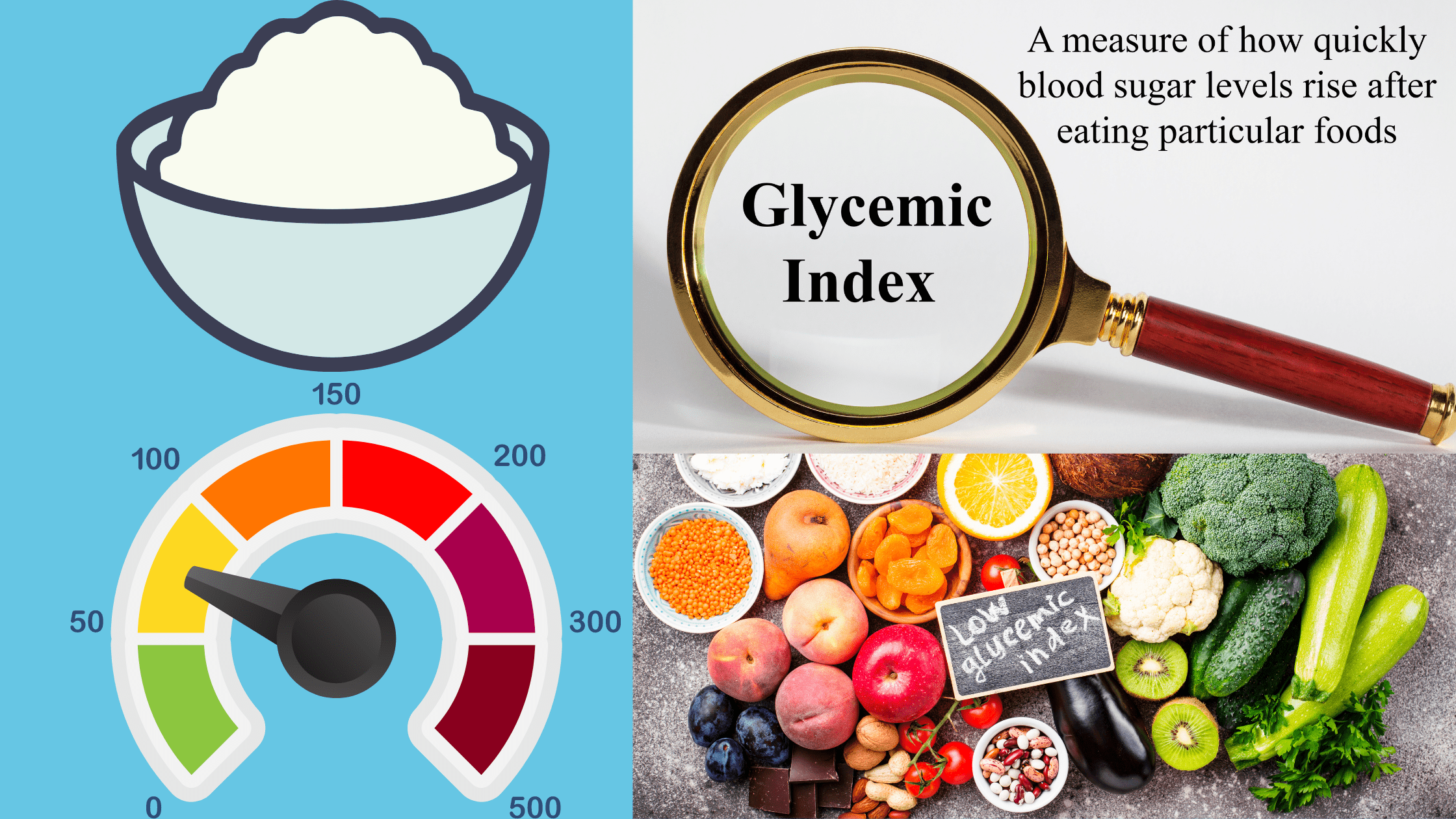
The duration and intensity of hyperglycemia and metabolic syndrome are the two essential risk factors for developing diabetic neuropathy in patients with type 1 or 2 diabetes.
Hyperglycemia is excessively high blood sugar that overwhelms the system, while metabolic syndrome is a cluster of diseases that consist of hypertension, high cholesterol, obesity, and diabetes.
Question number 1: How does diabetes neuropathy develop?
In diabetes, a complex array of metabolic and vascular factors shift the balance between nerve fiber damage and repair work in favor of damage. In other words, the body generally tries to keep our nerves healthy by avoiding and repairing the damage. Nevertheless, the damage rate goes beyond the body’s capability to handle the repair in severe diabetes.
This process preferentially impacts the distal sensory and free fibers, resulting in the progressive loss of experience that underlies the medical symptoms of diabetic neuropathy.
Individuals with diabetes have excess flowing glucose and lipids, which overwhelm the regular cellular function resulting in nerve damage.
Question number 2: Can diabetes trigger nerve damage?
The answer is yes. If the person with diabetes has high blood sugar levels circulating in their bodies for a long time, people with diabetes can get nerve damage. Another word for nerve damage is “neuropathy.”.
Individuals with diabetes can get various kinds of nerve damage. The most typical type of nerve damage brought on by diabetes is called “polyneuropathy.”.
Question number 3: What are the symptoms of nerve damage caused by diabetes?
Nerve damage impacts the feet and toes typically first. Some individuals do not feel any signs; however, others can have symptoms that consist of:
Tingling or loss of sensation. Burning or pain, which is often even worse at rest or night. Uncomfortable or irritating feeling with light touches.
As nerve damage worsens, signs can advance from the feet up the legs. Some individuals might likewise begin to feel symptoms in their hands.
Question number 4: Is there a test for nerve damage brought on by diabetes?
Your medical care professional or endocrinologist can usually figure out if you have nerve damage by talking with you and doing an exam. Sometimes, a doctor will check to inspect how well an individual’s nerves are working. This test is called a nerve conduction study, and neurologists typically do it.
Question number 5: How does nerve damage lead to problems?
Nerve damage can result in problems since it can make people unable to feel discomfort in their feet.
Typically, people feel pain when they get a wound on their feet. The pain tells them that they need to treat their injury so that it can heal. However, without pain, individuals with nerve damage might not feel discomfort when their feet get injured. They might not even know they have an injury, so they may not treat it. The lack of treatment can cause the problem to get worse. For instance, a neglected wound can get infected and become an open sore.
Nerve damage can likewise cause issues with the feet, muscles, joints, and bones. With time, this can cause an individual’s foot to have an irregular shape.

Painful foot due to diabetic neuropathy
Question number 6: What can you do to avoid or treat diabetes neuropathy?
Control your blood glucose levels: Symptoms of pain and burning sometimes get better when blood sugar levels are under control. So, taking your medications, eating healthy food, exercising, and following up with your doctor are crucial.
Take special care of your feet: Taking care of your feet can avoid future issues. It can likewise include a moderate pain from developing into a severe one.
To take and safeguard care of your feet, you can:
Wear slippers or shoes all the time. Never go barefoot.
Trim your toenails thoroughly. Do not cut cuticles or pop blisters. Ask your physician to do any procedures, including cutting the skin, such as removing an ingrown toenail.
Wash your feet with warm water and soap daily and pat them dry. Put a hydrating cream or lotion on the tops and bottoms of your feet.
Check both feet every day. Try to find cuts, blisters, swelling, or soreness. Make sure to inspect all over your feet, including between your toes. If you can not see the bottoms of your feet, use a mirror or ask another person to inspect.
Wear socks that are not too tight, and change them daily. Use shoes that fit well but are not too tight
Examine inside your shoes before you put them on. Ensure there is nothing sharp within.
Question number 7: What is the treatment for neuropathy?
Discomfort management with particular medications: Doctors can prescribe various medicines to treat pain triggered by nerve damage. Commonly used drugs include Gabapentine or Lyrica. They generally work well for nerve-based pain.
Foot issues: Doctors can deal with foot problems with different treatments, depending upon the problem’s seriousness. This may consist of:
Cleaning the sore on the foot and removing any dead skin or tissue around it. Prescribing antibiotic medications in scenarios where there is a wound infection. Doing surgical treatment to amputate a toe or part of the foot.
Question number 8: How often should my medical professional check my feet?
Your doctor needs to do a complete check of your feet once a year. The doctor should also routinely look at your feet at every medical visit.
Concern number 9: Can nerve damage be prevented?
It is possible to prevent nerve damage in diabetes. If you have diabetes, some research studies recommend you can lower your danger of getting nerve damage by doing the following:
Keep your blood sugar levels as near to normal as possible.
Avoid smoking cigarettes because smoking can also damage nerves and blood vessels.
Attempt to slim down if you are obese. This will not only help avoid diabetic neuropathy but will also assist in improving or potentially reversing your diabetes neuropathy.
Keep hypertension under control by treating it because uncontrol blood pressure adds to metabolic syndrome and blood vessel and nerve damage.
Treat cholesterol and remain active through regular exercise.
If you have it, treat heart illness.
We hope this article gives you lots of value. If you have remarks or concerns, please leave them below so our community can benefit and learn more.
Until later on, Thank you for reading,